Are There Physician Compensation Gaps Between Academic and Community Physicians? New Analysis Offers Insight (Part 1)
Community and academic physicians increasingly work together in the same health system, with many health systems including an academic medical center (AMC) and its faculty practice plan (FPP). Approximately 20 percent of hospital mergers involve academic medical centers (AMCs) and non-academic providers—resulting in an increasingly blended physician workforce.
In this context, disparate physician compensation packages for academic vs. community physicians have the potential to create friction, and to lead to increasing costs for AMCs and the systems of which they are a part. To assess the size and trend in compensation gaps, Veralon reviewed compensation data for 12 specialties, from the American Medical Group Association (AMGA) and Association of American Medical Colleges for 2014-2022. In Part 1 of this blog, we look at findings for eight non-surgical specialties. Part 2, to follow, will address the surgical specialties.
It’s natural to assume that the increasingly blended workforce is reducing the gaps in compensation between academic and community physicians. When Veralon undertook this analysis, we anticipated that while non-academic physicians may have earned significantly more than academic physicians in the past, mergers between AMCs and community hospitals would have led physician compensation levels to converge.
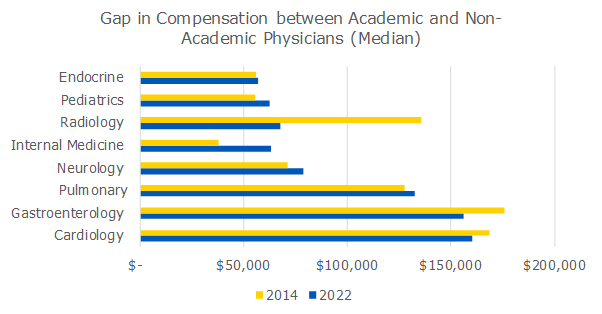
The data shows that this is not entirely the case; compensation has converged to some degree for some specialties but not for others. In the eight non-surgical specialties we reviewed, the 2022 compensation gap between academic and non-academic physicians ranged from $56,000 in endocrinology to $160,000 in cardiology.
For example, in 2014, AAMC reported median compensation of $284,000 for general cardiology associate professors , compared with AMGA reported median compensation of $452,000 for a general cardiologist (a gap of $168,000, with non-academic compensation 59% higher). By 2022 the gap had narrowed slightly but was still material at $160,000–40 percent higher for non-academic cardiologists. Interestingly, the gap narrowed because average annual academic compensation increased 4 percent per year compared to a CAGR of 2 percent in the AMGA data.
In contrast, the difference in compensation between academic and community radiologists declined from $135,000 in 2014 to about $67,000 in 2022.
Exhibit 1 shows the 2014 and 2022 compensation gaps for the eight non-surgical specialties.
Exhibit 1
Source: Veralon analysis of 2014-2022 median compensation market data. Academic data from American Association of Medical Colleges (AAMC) and non-academic data form American Medical Group Association (AMGA).
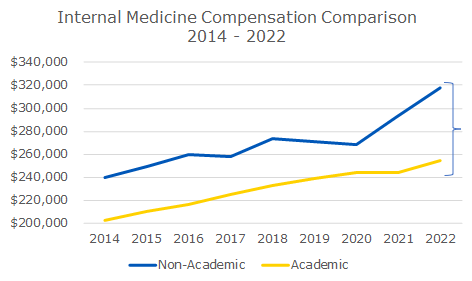
Unlike the other medical specialties, the compensation gap in internal medicine, while smaller than that in some other non-surgical specialties, is actually growing, as can been seen in Exhibit 2. It increased from $38,000 in 2014 to $63,000 in 2022, with academic compensation falling from 85 percent to 80 percent of non-academic compensation.
Exhibit 2
Source: Veralon analysis of 2014-2022 median compensation market data. Academic data from American Association of Medical Colleges (AAMC) and non-academic data form American Medical Group Association (AGMA).
Interestingly, during this time, the average annual growth in internal medicine compensation was 3.6 percent in the non-academic setting and 2.9 percent in the academic setting. We can likely attribute this difference to the central role primary care physicians play in the community hospital system, the shortage of primary care physicians and the challenging recruitment process.
Rate of Change
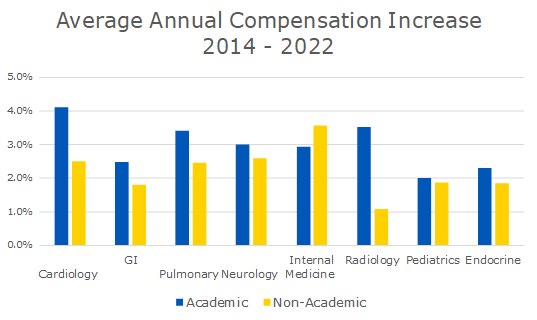
While the gaps in compensation between academic and non-academic physicians may not have consistently converged across the eight specialties reviewed, Exhibit 3 indicates that with the exception of Internal Medicine, average annual compensation increases in the academic setting outpaced those in the non-academic setting.
Exhibit 3
Source: Veralon analysis of 2014-2022 median compensation market data. Academic data from American Association of Medical Colleges (AAMC) and non-academic data from American Medical Group Association (AGMA).
Considering the Implications
The greater compensation increases in the academic setting are clearly a result of the aggressive recruiting required to enlist and retain AMC physicians and the potential competition between AMCs and their non-academic counterparts. It also means higher costs for AMCs.
We’ve seen this dynamic play out on the east coast, where one large health system integrated its academic and community physicians into a single medical group. To ensure there would not be internal equity issues between physicians at the academic medical center and physicians across the enterprise, the compensation models of these once-separate entities began to reflect a single-system model within specialties. The academic physicians received material pay increases.
In another case, an AMC acquired a community cardiology practice. Shortly thereafter, the faculty cardiologists demanded the same clinical compensation as their community counterparts, resulting in a huge cost increase for the AMC.
It appears that academic physicians may fall into two categories—those in specialties that are important to the AMC role as a tertiary center (who directly or indirectly contribute to bringing patients in and to the bottom line—and those in other specialties. These latter don’t have the leverage to overcome leadership cost control desires.
For non-surgical specialties, where compensation gaps are significant, health system leaders need to be prepared to respond to issues of pay equity—especially when younger, non-academic physicians are making substantially more than a long-tenured academic medical physician. Achieving systemwide collaboration—critical to meeting strategic goals in a tumultuous environment—depends on pay parity for physicians.
Compensation should never be a barrier to physicians working together and in collaboration with leaders to achieve an organization’s objectives. As more AMCs integrate with community hospitals and health systems, leaders must pay careful attention to where significant gaps in physician compensation exist and work to address them for the long-term health of the enterprise. This may be an expensive proposition.
Contact the Author:
Karin Chernoff Kaplan, Managing Director, kkaplan@veralon.com