Advanced Practice Clinicians in Medical Staff Planning: Four Factors to Consider
The growth and aging of the U.S. population will significantly increase the demand for medical care over the coming decade. At the same time, the supply of physician services is decreasing as physicians work fewer hours per week, and retirements are likely as more than a third of currently active physicians reach age 65 within the next decade.[1]
The supply of Advanced Practice Clinicians (APCs), in contrast, will grow over 40% between 2016 and 2030 according to some projections, and there may well be one APC to every two physicians by that year.[2] It is important to consider the potential need for and utilization of APCs when creating medical staff development plans.
Quantifying the need for APCs is as much art as science. Keep these factors in mind when considering how APCs can fit into your medical staff plan.
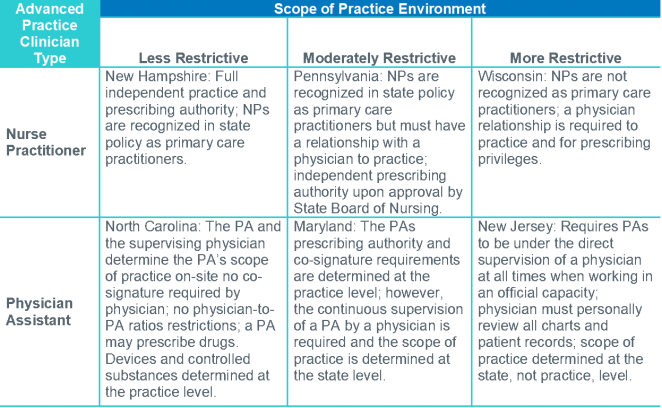
- The roles APCs can play are constrained by the scope-of-practice regulations in your organization’s state(s). For example, in 24 states, nurse practitioners (NPs) and certified nurse-midwives (CNMs) can establish independent practices, while in others a relationship with a physician is required for some aspect of the practice, such as prescribing or admitting patients to a hospital. (Certified Nurse Anesthetists have a different role and are not addressed in this article). In most cases physician assistants (PAs) must practice under the supervision of a physician, although the degree of autonomy can vary.
Exhibit 1 provides examples of more and less restrictive state practice provisions for NPs and PAs. It’s essential to understand the scope-of-practice rules in your state, and their implications for how APCs can be used within your clinical staff.
 1.Scope of Practice Policy, “Physician Assistants Overview.” http://scopeofpracticepolicy.org/practitioners/physician-assistants/. Accessed November 12, 2018.
1.Scope of Practice Policy, “Physician Assistants Overview.” http://scopeofpracticepolicy.org/practitioners/physician-assistants/. Accessed November 12, 2018.
2.American Academy of Physician Assistants, “State Laws and Regulations.” https://www.aapa.org/advocacy-central/state-advocacy/state-laws-and-regulations. Accessed November 12, 2018.
3.American Association of Nurse Practitioners, “State Practice Environment.” https://www.aanp.org/advocacy/state/state-practice-environment. Accessed November 12, 2018.
- Reimbursement for APCs varies with the role they play in a practice. When APCs practice independently, Medicare reimburses them at 85% of the physician rate. Given the already low margins on physician Medicare rates, this limits the situations in which true independent practice will make financial sense for APCs, even where allowed under scope-of-practice regulations. It probably does not make sense for systems or hospitals to set up independent practices for APCs.
In contrast, when APCs are billing “incident to” physician services—implementing a physician’s treatment plan—they are reimbursed at 100% of what a physician would receive for a visit. By using APCs in that role, hospitals and systems can empower physicians to work at the top of their license more of the time.
Private payers often follow Medicare’s lead. Medicaid policy varies; in most states it covers between 75% and 100% of the physician fee schedule payment.
- APCs can take on a range of important roles within physician practices. APCs can work with a great deal of independence within practices in most states. They can act as care managers or supervise them, supporting population health initiatives and improving care of patients with chronic health conditions.
APCs can improve care quality and patient satisfaction by helping practices reduce waiting times to get an appointment, improving decision-making, and reducing patients visits to the emergency room. In many cases they are able to spend more time with patients than physicians can.
Most NPs work in primary care of one form or another. In contrast, about two-thirds of PAs have roles in specialty practices, including internal medicine and surgery and their sub-specialties.[3]
- Look at the whole picture to decide how many APCs you need, and where. While it is possible to look at ratios of each type of APC to population and to the number of physicians, it may be difficult to develop a local inventory of APCs. Given the rapidly increasing supply of APCs, the ratios will in any case be changing significantly. APC to population ratios are likely to be lower in states where scope-of-service regulations are more limiting. These factors make it challenging to quantify specific need figures for APCs.
Another way to approach need is to start by looking at gaps in physician availability. Then consider how much of that unmet need should or could be filled by APCs. Surveys show that patients are highly satisfied with APCs, so this will not in most cases be a limiting factor. Physicians who do not have experience working with APCs, however, may not be fully comfortable with the idea of recruiting more than a few.
Ultimately, how many APCs you should recruit to fill gaps in physician availability will depend on:
- The scope-of-practice regulations for NPs, CNMs, and PAs in your state, as compared with full practice states.
- The need to adjust visit lengths; NPs will tend to spend a little longer with patients, and that is part of their attractiveness to patients. Their lower salary when compared with physicians makes this affordable. Assuming a 15 to 20 percent longer visit duration should be adequate.
- The clinical specialties where there are gaps in physician supply, e.g., a surgical PA can only complement a surgeon, a CNM needs minimal physician supervision, while in some states NPs can deliver primary care independently.
- Variation in the practice situations in which APCs might work; some situations will work better than others. Take into account the attitudes towards and experience with APCs of your existing medical staff, and if necessary, proceed with caution.
In a market with a shortage of physicians and an increasing number of APCs, there is no question that APCs can help health systems and hospitals meet clinical needs in their communities and for their medical staff. There is no fixed equivalency between a physician and a certain number of APCs; what is important is identifying where and how APCs can be used most effectively, which varies by market. In any case, APCs can make a valuable contribution to meeting identified community needs.
[1] 2018 Update: The Complexities of Physician Supply and Demand: Projections from 2016 to 2030, Final Report. Prepared for Association of American Medical Colleges.
[2] David I. Auerbach, PhD, Douglas O. Staiger, PhD & Peter I. Buerhaus, PhD, RN, Growing Ranks of Advanced Practice Clinicians—Implication for the Physician Workforce. NEJM Catalyst, August 2018,
[3] 2017 Statistical Profile of Certified Physician Assistants, National Commission on Certification of Physician Assistants. http://prodcmsstoragesa.blob.core.windows.net/uploads/files/2017StatisticalProfileofCertifiedPhysicianAssistants%206.27.pdf