The Bundled Care Pilot—Who is Participating, and How?
The pilot phase of the Bundled Payment for Care Improvement (BPCI) initiative has attracted 467 participants, according to the Centers for Medicare and Medicaid Innovation (CMMI). The great majority of these organizations will probably continue to participate when the performance period begins around July. BPCI offers these organizations an opportunity to learn how to better manage quality and cost across settings and encourages participants to share incentives with aligned physicians.
Looking at the participants, we note four points of particular interest:
- The preponderance (almost 80 percent) selected models in which providers continue to get paid the same way as always.
- Many (40 percent) are located in the Northeast (again expected). Although the number of participants in the West is low, it is possible that many of these organizations have undertaken more far-reaching risk-sharing deals, such as Medicare Advantage plans and Pioneer ACOs.
- Surprisingly, over 50 percent of participants selected more than 10 of the 48 MS-DRG “family” episodes CMMI identified, suggesting that many organizations are interested in more than just dipping their toe into the waters of bundled payment; however, they can still reduce the number of conditions or drop their participation altogether.
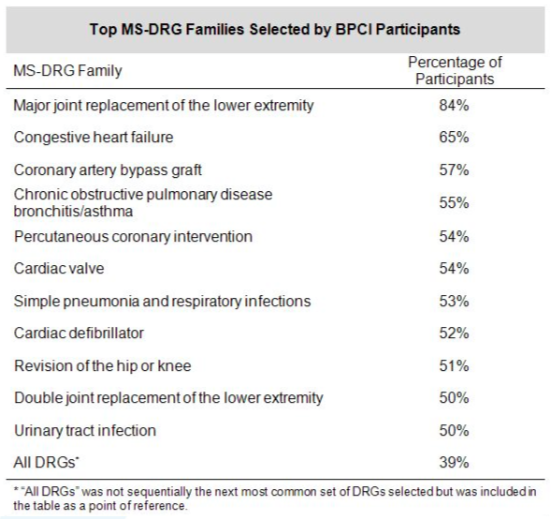
- Although most participants are interested in hip and knee replacements, the other MS-DRG families selected are more diverse, as evidenced in the exhibit.
Source: Veralon analysis of BPCI participants published by the Centers for Medicare and Medicaid Innovation; 2/11/2013
To help organizations identify areas of opportunity in episode management, improve quality, monitor partners, and track their costs across the performance period, BPCI pilot participants will receive Medicare claims data for their relevant episodes. Managing these data will not be easy. Participants will need to combine Medicare claims data with data from cost, financial, quality and other existing data systems. Finance leaders will need to ensure they have the resources in place to make this possible. The effort involved to accomplish this task hints at what will in all probability increasingly be required of healthcare provider organizations as the industry evolves under healthcare reform and the transition to value-based payment.
CMMI is expected to announce additional bundled payment models for chronic care in the near future. Medicare will eventually implement the National Pilot Program on Payment Bundling on a much larger scale. With current participation rates, bundled payments appear here to stay.