Continuing to Navigate the Changes in the Medicare Physician Fee Schedule
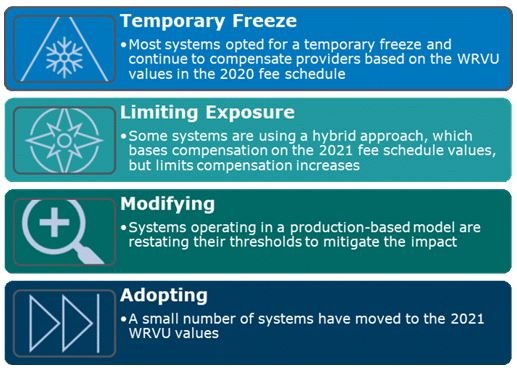
The changes in Work RVU (WRVU) values contained in the 2021 Medicare Physician Fee Schedule have the potential for wholesale disruption to productivity-based physician compensation models. To date, the response has varied among health systems, but for the most part, due to pandemic distractions and the sheer complexity of the impact, organizations have kicked the can down the road.
Those that are calculating the potential compensation impact without modifications to the comp models are learning that it is an expensive proposition with expense increases far outpacing revenue increases. Systems cannot wait to deal with this issue. The following graphic contains a summary of the estimated WRVU and Medicare revenue impact for common specialties.
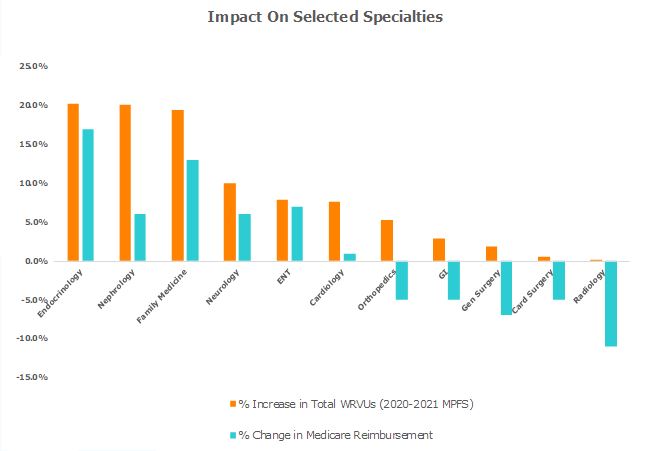
Consider a primary care physician with a base compensation of $220,000 and a compensation per WRVU rate of $50. Under the 2021 fee schedule, without any modifications to the compensation plan, the physician will earn $60,000 in additional compensation (approximately 20 percent), while the organization will collect, based on a Medicare payer mix of approximately 30 percent, an additional $20,000 or approximately 4 percent. In orthopedics, while WRVUs will increase approximately 5 percent, Medicare revenue will decline by 5 percent, and with a 30 percent Medicare payer mix, overall revenue will decrease by an estimated 1.5 percent.
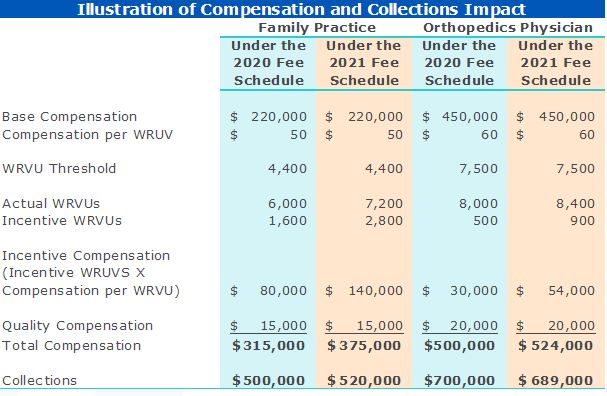
This expenditure increase without a corresponding revenue increase is not palatable nor tolerable for most institutions.
Due to the mix of responses by employers, and the time lag of the surveys, we do not believe the long-term impact of these changes will appear in the market data for at least two to three years.
The time is now to proactively develop a long-term solution. Responding will require facing some tough questions:
- CMS has essentially revalued physician services, placing more value on cognitive specialties and less on procedural specialties. Do we as an institution want to incorporate this foundational change into our compensation construct?
- Are there changes we can make to our current models that will reflect the revaluing of services?
- How can we minimize the financial impact to the organization? Do we want compensation in total to remain the same for the same services?
- If there is no budget for compensation increases, how do we respond to physicians in the cognitive specialties, who believe they should be compensated more?
- Are our commercial payer contracts based on Medicare payment rates and, if so, how soon will commercial payments be affected?
- Given the disruption this change caused in our compensation models, do we want to decrease the emphasis on WRVUS in our compensation models?
Choosing the optimal direction will require consideration of these challenging questions as well as contractual obligations, potential fair market value and commercial reasonableness issues and internal group equity.
Material expense increases without offsetting increases in revenue will prove unsustainable, thus doing nothing is definitely not an alternative.